Accessibility Statement
Stories
Prioritizing Health in a New Era of Type 2 Diabetes Care
Diabetes Project in Indianapolis Showcases Impact of Community Health Workers
Advocating for Inclusive Obesity Care
Identifying Drivers and Barriers to Anti-Obesity Medication Use in Obesity Care
Bridging the Gap Between Biomarker Testing and Treatment
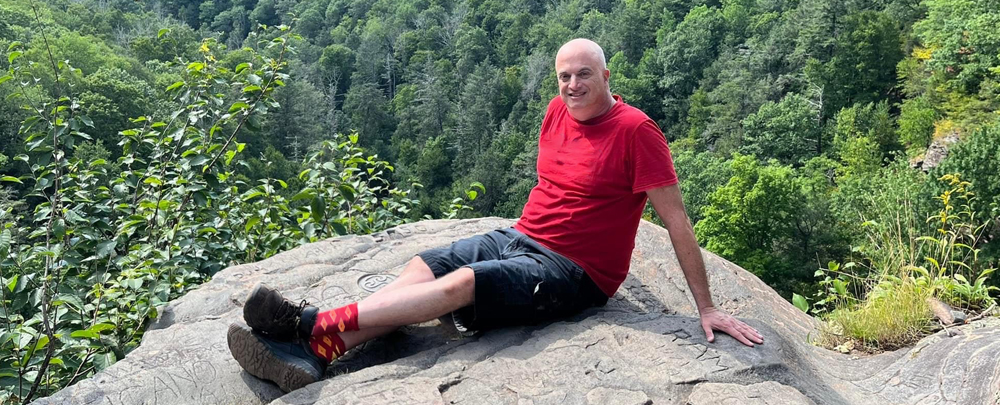
Support Is Everything: Brian’s Mantle Cell Lymphoma Journey
Solar Energy Structures Planned for Indianapolis Headquarters
MCL Treatments Have Come a Long Way — But Patients Who Relapse Still Need More Options
Taking on a Disease That Can't Be Ignored